
A sleep study is called Polysomnography (PSG). A home sleep study is called an Ambulatory Polysomnography Test. We work collaboratively with Sleep Better Again, a National company specializing in Home Sleep Studies.
A home Home Sleep Study (HSS) sometimes called a Home Sleep Test (HST) is a convenient but effective way to investigate the quality of your sleep and screen you for any sleep related issues like snoring and obstructive sleep apnoea. During this process certain vital signs are measured such as your heart rate, respiratory rate, breathing patterns and effort, oxygen levels, sleep staging, as well any teeth clenching or grinding.
There are various signs and symptoms you may be aware of which can alert you to suspect an issue with your sleep. These include but are not limited to:
Other associated issues may be:
The sleep study is carried out in the comfort of your own home and bed. On the nominated night, you will wear the sleep study device to bed. You will be shown how to attach the various leads and sticky electrodes to your head and face during our Sleep Study Set-Up Consultation the day of your sleep study. The Sleep Study measuring device (about the size of a smartphone) is kept strapped to your chest. The device is pre-programmed during your consultation to switch on at a certain time based on when you normally go to bed. During the night the device will record all the relevant information about your sleep patterns and quality. It will also record any teeth clenching or grinding which is very commonly experienced by sufferers of sleep apnoea (as the body repetitively moves the jaw in an effort to open up the airway to help you get more oxygen.)
Upon returning the device the next morning, the recorded data from the device is then uploaded for analysis. As mandated in Australia, all sleep study data is analyzed by an Independent registered Sleep Physician who will then make a formal diagnosis as to if you have any sleep apnoea and the severity.
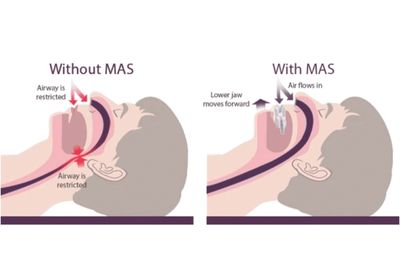
Mild to moderate sleep apnoea and snoring is best treated with a specialised splint (bite plate) called a Mandibular Advancement Splint (MAS). This splint is customized for you by first taking a detailed 3D scan of your mouth and teeth following which the data is sent to a lab for manufacture. The MAS has a top and bottom piece that fits on your teeth, and is designed to pull (advance) your bottom jaw (mandible) forwards to open up your airway.
Severe sleep apnoea is sometimes treated by a CPAP machine. This requires you to wear a mask which is attached to the machine. The machine generated a continuous positive airway pressure keeping your airway open. Sometimes people cannot tolerate a CPAP and will opt for a MAS instead.
Addressing other associated issues is also an important part of treatment. These include weight loss if required, doing regular exercise, and adopting better sleep hygiene habits (night time habits).
While sleep apnoea and TMD are separate conditions, there is evidence to suggest that they can be linked. One study found that people with TMD were more likely to also have sleep apnoea than people without TMD. This is thought to be because TMD can cause changes in the structure of the upper airway, which can increase the risk of airway obstruction and, therefore, sleep apnoea Conversely, sleep apnoea may also contribute to TMD. This is because the repeated episodes of breathing pauses and gasping for air can cause muscle tension in the jaw and face, leading to jaw pain and other TMD symptoms. Clenching and grinding, can be symptoms common to both.
Additionally, it is important to ensure that when beginning to use as MAS, that this does not lead to discomfort in the jaw, neck or head. Other symptoms to watch out for are earache, blocking or ringing. These may all be signs that your joints and muscles are stiff / tight and require treatment so that you can wear your MAS without any issues.
Next Steps
For Rapid Relief & Lasting Results Call (03) 9824 8868
(03) 9824 8868
OrClick Here to Book Online